Telehealth for Libraries Guide Report
Libraries on the vanguard of transforming healthcare delivery, what is your library going to do in this moment when the federal government is committing over $7 billion to communities making a difference?
This guide lays out how to a) get to the heart of patrons’ healthcare needs, b) create something that’s never been done in your community before, and c) market your telehealth and broadband grant proposal.
More than video chats, telehealth uses intranets and Internet networks to observe, diagnose, initiate or otherwise medically intervene, administer, monitor, record, and/or report on the continuum of care people receive when ill, injured, or wanting to stay well.
I’ll take this definition one step further and differentiate between
1) real-time telehealth,
2) store-and-forward telehealth, and
3) “passive” telehealth.
Real-time telehealth are activities happening “right here and now,” often involving medical or healthcare professionals. In a library setting, a patron is video chatting with a doctor from a study room or other enclosed private space, or a traveling nurse sets up in a room to do hypertension screening with patrons and video conferencing with a doctor in another location should patrons have questions.
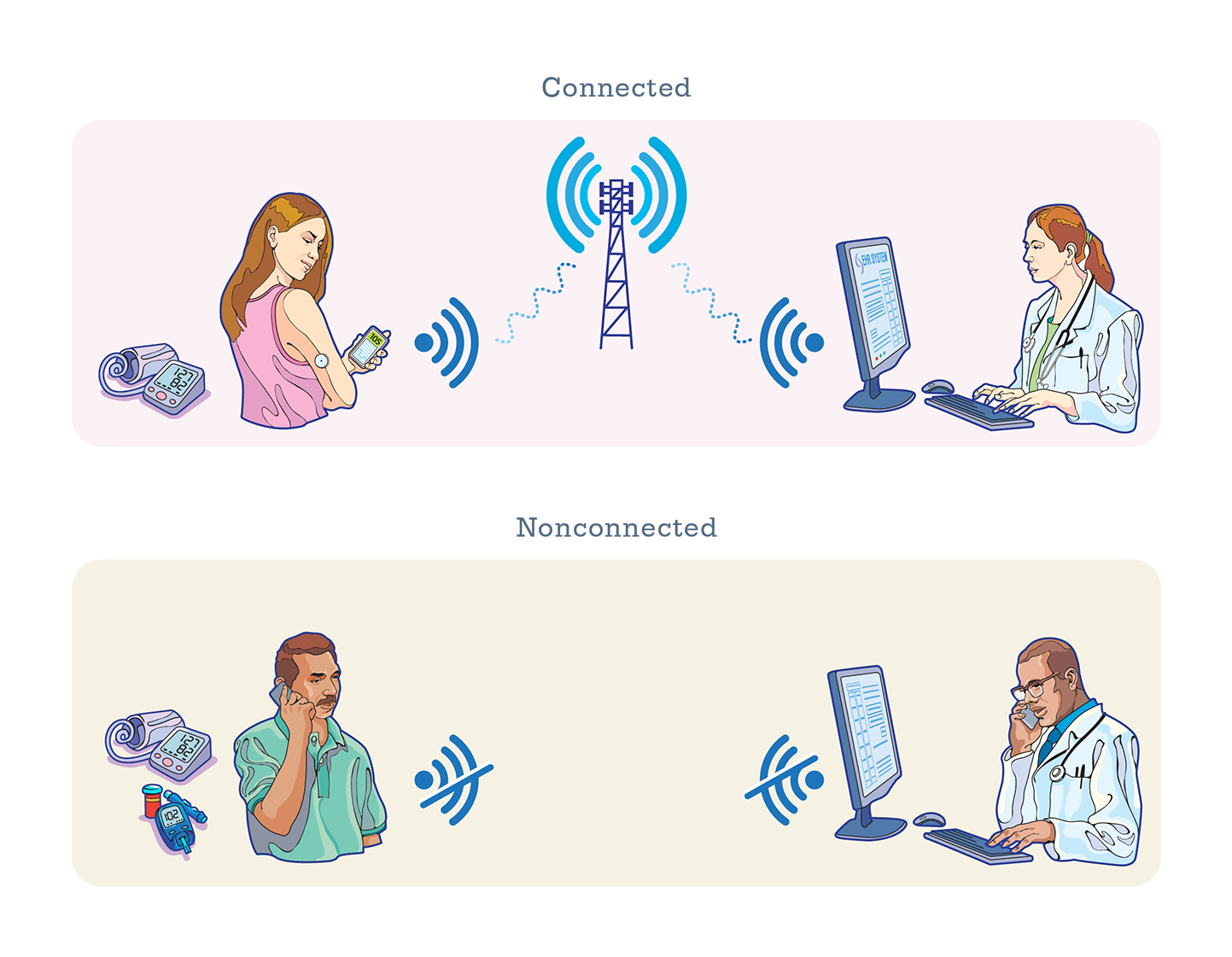
Store-and-forward telehealth is collecting medical data and sending it electronically to another site for later evaluation. Patrons who don’t want to go over their data cap (limit) might use a library’s Wi-Fi to send medical records, test results, or digital images. For maximum privacy and security, telehealth applications receive and send using HIPAA-compliant software.
In the context of this guide, “passive” telehealth refers to educational Web content, digital knowledgebases, and software applications that help us understand, prevent, treat, or recover from threats to our physical and mental health. Few entities are as competent as libraries for making knowledge easy to find and sort through.
Telehealth making a difference
There are at least five primary ways to impact healthcare delivery through telehealth at libraries:
1. Reinventing the doctor office visit – video consults for a variety of healthcare practices including observation, screening, gathering body data, data exchange, counseling
2. Marrying chronic healthcare and home care – libraries can check out Wi-Fi hotspots and laptops to patrons, plus add exciting, interactive Web content
3. Aiding emergency response – turning libraries into wireless way-stations to connect ambulance crews en route from rural homes to far-off hospitals
4. Expanding mental health care – in addition to the video consult, there can be interactive content, in-person group sessions, and meetings with social workers
5. Improving senior care and aging in place – another benefit of checking out portable hotspots
“If the overall strategy is to make telehealth a part of 21st-century cities and rural living, if it’s part of our vision that ‘Telehealth is the future of healthcare,’ we’re going to have to come up with lots of different ways to reach lots of different communities,” said Francella Ochillo, Executive Director of Next Century Cities. Libraries supporting telehealth in laundromats, barbershops, and hairdressers is part of that strategy.
This guide lays out a straightforward needs assessment process so you get a representative portrait of how telehealth can benefit the community. Libraries reach out and touch virtually everyone in their communities across the entire economic spectrum, so it’s quite exciting to imagine telehealth capabilities at work.
Healthcare professionals weigh in on how to get the maximum impact from telehealth
technology in your library. The guide also gives you tips and pointers on getting the best from your IT investment. Not only does it address access to broadband but also broadband and telehealth adoption and training.
Ultimately, it takes funding to transform community dreams into reality. The guide offers insights into federal grant programs that fund libraries and telehealth: the FCC’s E-rate program, the Institute for Museums and Library Services (IMLS), and Health & Human Services (HHS), plus links to other valuable resources that help you.
For the full report download the pdf for free without registration — 2021 05 LibraryTelehealthGuide